ORTHOSTATIC INTOLERANCE
Orthostatic intolerance is a broad term that refers to a spectrum of dysautonomic disorders, including Postural Orthostatic Tachycardia Syndrome (POTS) and Orthostatic Hypotension (OH). A key feature of orthostatic intolerance is the appearance of symptoms upon standing.
In the case of Orthostatic Hypotension (OH), blood pressure drops by 20 mmHg or more, or diastolic blood pressure decreases by 10 mmHg within 3 minutes of standing. This can last for several minutes and usually resolves on its own or with a change of position. Along with the drop in blood pressure, the following symptoms may occur:
- Dizziness or spinning sensations
- Blurred vision
- General weakness
- Fainting or feeling like you are about to faint
- Confusion
Orthostatic hypotension has been observed to be more common in the elderly.
OH is divided into neurogenic and non-neurogenic OH. Neurogenic OH is associated with neurodegenerative disorders (such as multisystem atrophy and Parkinson’s disease), autoimmune diseases, and neuropathy-related conditions such as diabetes mellitus. When standing, the volume of circulating blood decreases by approximately 500-1000 ml. Reduced blood volume lowers blood pressure. When baroreceptors sense reduced stretch due to reduced intravascular volume, compensatory mechanisms increase heart rate and vascular tone to reduce the effects of reduced circulating blood volume. In orthostatic hypotension of neurogenic origin, due to impaired release of norepinephrine, there is no increase in vascular tone after standing up, resulting in a drop in blood pressure and the above-mentioned symptoms.
Neurogenic OH is caused by different mechanisms, including a decrease in circulating blood volume or induced by diuretics (stimulating urine output) and vasodilators.
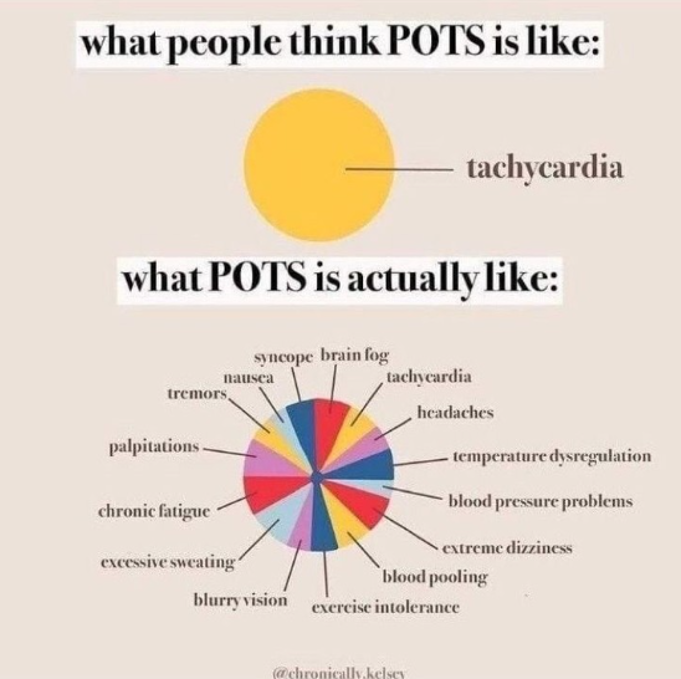
Postural orthostatic tachycardia syndrome (POTS) is defined as a persistent increase in heart rate of 30 beats per minute (40 bpm in children) or more after a 10-minute change from supine to standing or sitting in the absence of OH. A heart rate of 120 bpm is commonly observed in POTS patients after repositioning. POTS primarily affects women of childbearing age. Patients with POTS and OH report debilitating symptoms including dizziness, tachycardia, presyncope, nausea, headache, difficulty concentrating, and memory problems.
Theoretically, POTS is the culmination of several underlying pathological processes, including peripheral neuropathy/denervation, hypovolemia with altered renin and aldosterone levels, and a hyperadrenergic state.
An association between autoimmune diseases and orthostatic intolerance has been observed. Cases of patients with autoimmune OH have been published. In addition, about 20% of POTS patients have been diagnosed with commobid autoimmune disease (Hashimoto’s thyroiditis, celiac disease, Sjogren’s syndrome, rheumatoid arthritis, systemic lupus erythematosus, etc.).
Many patients with POTS complain of chronic fatigue (48%), sleep disturbances (32%) and myofascial pain (16%). The conditions of chronic fatigue syndrome and POTS often overlap. Patients with POTS and chronic fatigue syndrome have higher laboratory markers of sympathetic activation than patients without chronic fatigue.
The COVID-19 pandemic has generally been associated with respiratory symptoms in the acute phase, but there has been a variety of symptoms associated with subacute COVID-19 infection. Long COVID is a term that includes ongoing symptomatic COVID-19 illness (4-12 weeks) and post-COVID-19 illness syndrome (> 12 weeks) that are not explained by an alternative diagnosis. Case studies describe the new onset of symptoms of autonomic dysfunction with evidence of POTS/inappropriate sinus tachycardia in the subacute phase of COVID-19 infection. The underlying cause of dysautonomia following COVID-19 infection is not well understood. However, SARS-CoV-2 viral infection, which induces an autoimmune response and direct neurotoxic effects, was thought to be the main cause of the development of POTS after COVID-19. Wallukat et al. conducted a study that examined 31 patients with POTS and COVID-19.
The diagnosis of orthostasis intolerance is used:
- Questionnaires (COMPASS-31, Malmo POTS score)
First, the patient is interviewed in order to find out whether the symptoms he is experiencing are typical of orthostasis intolerance. Standardized questionnaires are most often used, which can also be completed online.
COMPASS-31 questionnaire to assess different functions. A score of 20 or more is likely to be at moderate risk for POTS syndrome.
https://www.hattrevaluationtools.eu/compass-31/ (test can be taken here)
The Malmo POTS Calculator helps you assess your symptoms. A score of 42 or higher indicates a probable diagnosis of POTS.
https://www.standinguptopots.org/MalmoPOTSscore (test can be taken here)
- Passive orthostasis test
A special TILT TABLE test device is used for this. The patient lies down on a special medical couch with safety belts and leg support. Connects to electrocardiogram (ECG), blood pressure and pulse monitors. The couch is then raised to a near standing position (70 degrees vertical to simulate standing up from a lying position.
The test measures blood pressure, heart rate and an electrocardiogram (ECG) to assess changes in position. Various symptoms may appear during the test (dizziness, ringing in the ears, coughing, shortness of breath, trembling or sweating, skin color change, fainting, etc.).
- In the absence of a passive orthostasis test, the NASA lean test can be performed, which is performed using a blood pressure monitor and pulse oximeter. During this test, how the patient’s well-being and vital signs change after standing up and leaning their shoulders against the wall is monitored.
- Electrocardiogram (ECG) and Blood tests to rule out co-morbidities.
It is important to have an overall picture and assess whether the symptoms are not caused by other diseases (anemia, heart rhythm or conduction disorders, thyroid diseases, etc.).
TREATMENT
The initial approach to managing POTS/OH is usually non-pharmacological, including avoidance of triggers (heat exposure and prolonged standing), gradual exercise training, use of waist-high compression stockings, and ample salt and fluid intake. Fludrocortisone, ivabradine, beta-blockers, midodrine, and pyridostigmine may also be prescribed for additional treatment. These drugs can be used as monotherapy or, more commonly, as combination therapy. For medicinal treatment, it is necessary to consult a doctor.
- Regardless of the underlying pathophysiological mechanism, most patients need to increase their daily water intake (2-2.5 L).
- Excessive caffeine intake should be avoided as it increases diuresis and promotes hypovolemia.
- Increase your salt intake (up to 10 g/d depending on the severity of your symptoms). It helps raise blood pressure.
- Physical exercises. Vascular tone, muscle strength and the release of pain-relieving endorphins increase. Must be tailored to the specific needs of the patient. It is ideal to start working with a physical therapist. Increase the intensity very gradually. It is important that patients start with a lower load and increase it slowly. Lymphatic drainage pneumatic massage of the legs and abdomen can also be one of the methods.
- Nutrition recommendations. Some patients report improvement in symptoms following a gluten-free diet and/or a FODMAP (low-carb) diet.
- Compression socks. Reduces blood accumulation in the lower limbs. Can be used up to the groin or even covering the waist.
- Sleep hygiene. It is recommended to avoid stimulating screens at least 30 minutes before bedtime.
- Avoid alcohol. Alcohol can worsen symptoms in POTS patients. Alcohol causes dehydration and can increase hypotension due to venous dilation and should be avoided by most POTS patients.
- Avoid standing for long periods of time. It is important to avoid standing for long periods of time, as standing worsens POTS symptoms in most patients. If you have to stand for long periods of time, try flexing and squeezing the muscles in your feet, legs, and buttocks, or shift your weight from one foot to the other. The more you can move your lower half while standing, the better the blood will return to your heart.
WHEN to see a doctor?
- Severe and/or prolonged fatigue
- Dizziness when sitting or standing for a long time, which may cause fainting
- Feeling like you’re about to pass out after changing position
- Tinnitus, ear congestion, especially when changing position
- Brain fog: Difficulty concentrating, remembering, or concentrating
- Strong palpitations, especially when changing position from sitting to standing
- Nausea and vomiting
- Headaches
- Excessive sweating
- Trembling
- Shortness of breath
- Chest pain
- Flatulence
- Exercise intolerance or prolonged worsening of general symptoms after increased activity
- Pale face and purple hands and feet
- Sleep disorders
- Urinary disorders
- Visual disturbances
Symptoms usually intensify:
- In a warm environment, such as a hot bath or shower, a hot room, or on a hot day
- In situations where there is a lot of standing, such as waiting for a bus or shopping
References:
- “Autoimmunity in Syndromes of Orthostatic Intolerance: An Updated Review”, Clarissa Pena, Abdelmoniem Moustafa , Abdel-Rhman Mohamed and Blair Grubb, 20 April 2024, Journal of personalized medicine.
- https://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/symptoms-causes/syc-20352548
- https://www.mayoclinic.org/diseases-conditions/orthostatic-hypotension/diagnosis-treatment/drc-20352553
- https://www.sciencedirect.com/science/article/abs/pii/S1566070218300523
- https://www.standinguptopots.org/MalmoPOTSscore
- https://www.hattrevaluationtools.eu/compass-31/
- https://pubmed.ncbi.nlm.nih.gov/23218087/
- https://www.mayoclinicproceedings.org/article/S0025-6196(12)00896-8/pdf
- https://www.ahajournals.org/doi/pdf/10.1161/JAHA.120.017610
- https://www.sciencedirect.com/science/article/pii/S0735109720379079
- https://thedysautonomiaproject.org/dysautonomia/
ANTALGIJA reabilitacija Jums
Klinika ANTALGIJA – tai reabilitacijos įstaiga, kuri teikia mokamas nervų sistemos ligų, judamojo-atramos aparato pažeidimų ambulatorinės medicininės reabilitacijos, šeimos medicinos paslaugas.
Šiame puslapyje skelbiama informacija skirta tik švietimo tikslais. Remiantis ja,- neturėtų būti diagnozuojamos ligos/disfunkcijos ar priimami sprendimai dėl konkretaus gydymo, tai turi būti atliekama tik konsultuojantis su kvalifikuotu sveikatos priežiūros specialistu.






